❖ Introduction:
Each year, more than 100000 women in India alone receive a breast cancer diagnosis. Each year, the disease claims the lives of about 10000 women. It is the most prevalent malignancy among women and the second-leading cause of cancer-related death, trailing only lung cancer. Although younger women are more likely to get breast cancer, elderly women are still at significantly higher risk. In 1998, there were 5% of instances identified in the women under the age of 35, 30% in those between the ages of 35 and 49, 31% in those between the ages of 50 and 64, and 33% in those over the age of 65. The lifetime risk of breast cancer for women is roughly 13%. With a lifetime risk of more than 50%, around 0.1% of women have a hereditary mutation in the BRCA1 or BRCA2 breast/ovarian cancer susceptibility gene. The national average of cancer cases for 2022 is 100.4 per 100,000, with a large number of women (105.4 per 100,000) being diagnosed with breast cancer, a preventable disease. By comparison, 95.6 men per 100,000 have been diagnosed with lung cancer!
When age was taken into account, there was a very slight annual increase in breast cancer incidence from 1940 to the mid 1980s. Obtrusive bosom disease occurrence became by 3-4% each year all through the 1990s, for the most part because of the broad utilisation of screening mammography that began in the mid 1980s. Ductal carcinoma in situ (DCIS) rates developed by almost a component of six throughout this time, ascending from around 5 occurrences for every 100 000 ladies in 1980 to more than 30 for each 100 000 out of 1998. The age-changed pace of bosom disease mortality has fallen by around 2% every year during the 1990s, in spite of the way that bosom malignant growth frequency among ladies has expanded since the mid 1980s, and conceivably because of this increment.
Scientists regularly credit better bosom malignant growth therapy and expanded utilisation of evaluating mammography for this expansion in bosom disease endurance. Endeavours are being made to all the more obviously characterise the general effects of the factors influencing bosom disease endurance. During the 1980s and 1990s, a critical progression in bosom disease research had close to nothing to do with science. Solid promotion bunches that battled to propel bosom disease research were framed during these years. Beginning around 1990, government subsidizing has dramatically increased, and grass-roots activism has prompted an unmatched plan of financing for bosom malignant growth research that is directed by the Branch of Protection.
Also, patient backers are presently knowledgeable in research-related subjects, and a significant number of them regularly sit close by proficient researchers on legislative panels that direct how much cash ought to be spent on examination and what sorts of medicines ought to be suggested. Patient promoters likewise sit on institutional survey sheets, information well-being checking sheets, and helpful gathering boards that coordinate clinical investigations for bosom disease. To support the extent of ladies who participate in clinical preliminaries, promotion associations have worked. The Public Bosom Malignant growth Alliance Asset’s (NBCCF) Clinical Preliminary Drive (CTI) monitors clinical preliminaries and energizes individuals with bosom disease to select (see NBCCF). A clinical preliminary should address a critical, extraordinary examination issue connected to bosom malignant growth, be planned with logical thoroughness, and utilize OK and important results before it tends to be added to the NBCCF vault.
❖ Staging:
The size and different attributes of the primary growth (T), the state of the ipsilateral lymph hubs (N), and the presence or non-attendance of far off metastases (M) are utilized by the American Joint Panel on Disease (AJCC) and Singletary to organise bosom malignant growth. Blends of these TNM positions decide the ailment stage, which goes from 0 to IV. Ductal and lobular carcinoma in situ (DCIS, LCIS), which are non-invasive and potentially benign types of the disease, make up stage 0. The breast or its immediate surroundings are the only locations where the tumour can spread during stages I to III of the disease. Greater involvement of locoregional cancers or larger primary tumours are indicative with higher stages. Stage IV patients are those who have indications of distant metastasis. Depending on how the healthcare system handles diagnosis and reporting, the distribution of disease stages at the time of breast cancer diagnosis differs by nation. Approximately 21%, 42%, 29%, 5%, and 4% of women have been diagnosed with Stage 0 to Stage IV illness, respectively. Another approach of classifying tumours based on histopathologic analysis has low discriminatory power because infiltrating ductal carcinomas account for 70–80% of all cancers.
❖ Prognosis:
Breast cancer comes in various forms. Many breast cancers spread slowly, and those who have them live for many years before passing away from other reasons. By the time the main cancer is discovered, other, more aggressive tumours may already migrate to distant locations. The consequences of this heterogeneity for research at all stages of the disease, from screening and symptomatic procedures up to the appraisal of medicines for cutting edge sickness, are critical.
The most often recognised factor impacting patient results is stage. With a middle endurance season of 18 to two years, stage IV infection is regularly remembered to be serious. Notwithstanding, a minuscule level of people with stage IV sickness experience a total reduction in the wake of getting fundamental chemotherapy and proceed to live for a long time.
In any case, patients with Stage I sickness, which comprises of a little essential growth and no lymph hubs that have been impacted, have basically a 90% possibility remaining infection free following five years. Contribution of the lymph hubs is connected to a more terrible visualisation, with paces of infection free endurance for a very long time going from 50 to 75 percent. Menopausal status, growth grade, and proliferative movement are minuscule variables. In spite of being a critical prescient marker, stage limitedly affects how well a treatment will function. Albeit the outright advantage can be significantly higher for higher stage disease, the proportional advantages of treatment are generally similar throughout stages. The focus of a lot of current research is on variables that may indicate whether a certain treatment technique will be clinically effective (‘predictive factors’), as opposed to more traditional ‘prognostic factors,’ which are thought to be markers of overall tumour aggressiveness, regardless of kind of therapy. Oestrogen receptor (ER) status, a crucial predictor of how well a tumour will respond to hormone therapy, is the most thoroughly researched prognostic factor. According to the Early Breast Cancer Trialists’ Collaborative Group [EBCTCG], tamoxifen and other selective oestrogen-receptor modulators (SERMs) are extremely effective in treating hormone-sensitive breast cancer, but they are ineffective in treating progesterone- and ER-negative tumours. Aromatase inhibitors may be beneficial for patients who benefit from SERMs.
❖ Authentic Point of view on Clinical Preliminaries in Bosom Disease:
1. Medical procedure and Radiotherapy:
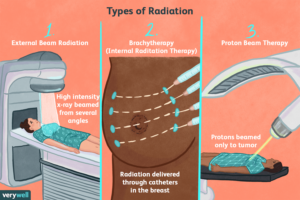
Over the most recent 50 years, there has been a huge change in how researchers figure out the science of bosom disease. Huge randomised preliminary discoveries have been a critical calculate of this change. Bosom malignant growth was accepted to be a neighbourhood/local sickness that proliferated straight forwardly along lymphatic pathways to far off regions from the nineteenth 100 years until the 1970s. The careful strategies upheld by W.S. Halsted at the turn of the twentieth hundred years, like significant resection of the bosom, local lymphatics, lymph hubs, and muscle were brought into the world from this thought.
All through the principal half of the 100 years, this surgery, known as an extreme mastectomy, stayed the fundamental technique for treating bosom disease, sporadically related to radiotherapy. During the 1960s, directing enormous scope randomised clinical preliminaries to look at elective treatment ignited banter among specialists in the field of bosom malignant growth as well as in other clinical strengths. A notable bosom disease specialist shot such discoveries as “an extraordinary jump in reverse in the therapy of bosom malignant growth” in a hostile discussion.
In spite of this obstruction, early scientists in the space continued making preliminaries to resolve critical restorative issues of the time, and they were additionally effective in persuading patients to participate in this state of the art idea of randomizing treatment. These fundamental examinations differentiated different careful and radiation methods. In an exploration led in 1971 on almost 1700 ladies, there were no way to see an endurance distinctions between standard radiotherapy, all out mastectomy with radiation, and complete mastectomy with axillary hub analisation.
Results from this examination and comparable ones directed at the time interrogated long-held hypotheses concerning the sickness and steadily convinced scientists that their thought that bosom malignant growth was a nearby infection best treated with forceful neighbourhood therapy techniques was off base. All things being equal, obviously bosom malignant growth was a fundamental condition that might profit from foundational treatment, and cruel neighbourhood treatments were not generally seen to be pivotal for expanding endurance.
2. Chemotherapy:
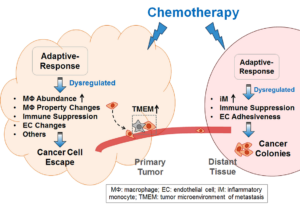
The principal cytotoxic medications for the treatment of strong cancers were made during the 1950s. At the point when utilised as single specialists in unassuming examinations, a few of these demonstrated to be extremely delicate to bosom malignant growth. Blends of these cytotoxic medications were in this manner examined, with the Cooper routine (cyclophosphamide, methotrexate, 5-fluorouracil, vincristine, and prednisone) being quite possibly of the earliest. The preparation for the fast improvement of adjuvant chemotherapy was laid during the 1970s with the presentation of bosom disease as a foundational sickness and the shown responsiveness of bosom malignant growth cells to cytotoxic medications. A randomised examination standing out a medical procedure from blend chemotherapy to medical procedure alone found that utilising this adjuvant treatment strategy could impressively bring down the gamble of illness repeat. Doxorubicin’s presentation as a therapy for bosom malignant growth fills in to act as an illustration of the various clinical preliminaries that are regularly led for the improvement of new medications. Right on time during the 1970s, little preliminaries in strong growths demonstrated portion and security; these were quickly trailed by Stage II preliminaries of the medication in metastatic bosom disease.
Doxorubicin was then tried in mix with different medicines, and randomised preliminaries exhibited that blends containing doxorubicin could bring about more prominent reaction rates in metastatic sickness. Following these accomplishments, different doxorubicin and other anthracycline-containing mixes were presented as adjuvant therapies for essential bosom disease. These mixes, in some cases alluded to by the abbreviations “FAC,” “CAF,” “FEC,” and “AC,” keep on being urgent in the administration of bosom cancer.22,23 Treatments containing anthracyclines further develop endurance in early bosom malignant growth and further cut the likelihood of repeat.