❖ Introduction
In the battle against bacterial infections, antibiotics have emerged as potent weapons that have transformed the landscape of modern medicine. As integral players in the field of pharmacy practice, antibiotics play a critical role in combating infections and saving lives. This comprehensive blog will delve deep into the world of antibiotics, exploring their historical significance, mechanisms of action, diverse classes, pivotal role in pharmacy practice, challenges posed by antibiotic resistance, and the imperative need for responsible antibiotic stewardship.
❖ Antibiotics: A Historical Perspective
Alexander Fleming
The discovery of antibiotics is a remarkable tale of scientific serendipity and visionary minds. In 1928, Alexander Fleming’s accidental observation of mold inhibiting bacterial growth marked the inception of antibiotics. This serendipitous discovery led to the development of penicillin, the first widely used antibiotic. Subsequent decades witnessed the isolation and production of various antibiotic classes, revolutionizing the treatment of infectious diseases and fundamentally altering the healthcare landscape.
❖ Mechanisms of Action: Bacterial Battleground
Antibiotics wage their war against bacteria through ingenious mechanisms that target specific vulnerabilities of these microorganisms. Understanding these mechanisms offers a glimpse into the intricacies of bacterial warfare:
- Cell Wall Disruption: Penicillins and cephalosporins disrupt bacterial cell wall synthesis, leading to weakened cell walls and eventual lysis.
- Protein Synthesis Inhibition: Antibiotics like macrolides, aminoglycosides, and tetracyclines interfere with bacterial protein synthesis, preventing the production of essential proteins required for bacterial growth.
- Nucleic Acid Interference: Fluoroquinolones and metronidazole disrupt bacterial DNA replication, inhibiting bacterial reproduction and propagation.
- Metabolic Pathway Blockade: Sulfonamides and trimethoprim inhibit key metabolic pathways, depriving bacteria of essential building blocks for growth.
❖ Diverse Classes of Antibiotics:
Antibiotics, the stalwarts of modern medicine, come in a diverse array of classes, each armed with unique mechanisms to combat bacterial infections. From disrupting cell walls to inhibiting protein synthesis, these classes represent a pharmacological arsenal that pharmacists wield to save lives and protect public health. Let’s explore some of the major classes of antibiotics and their mechanisms of action:
- Beta-Lactams:
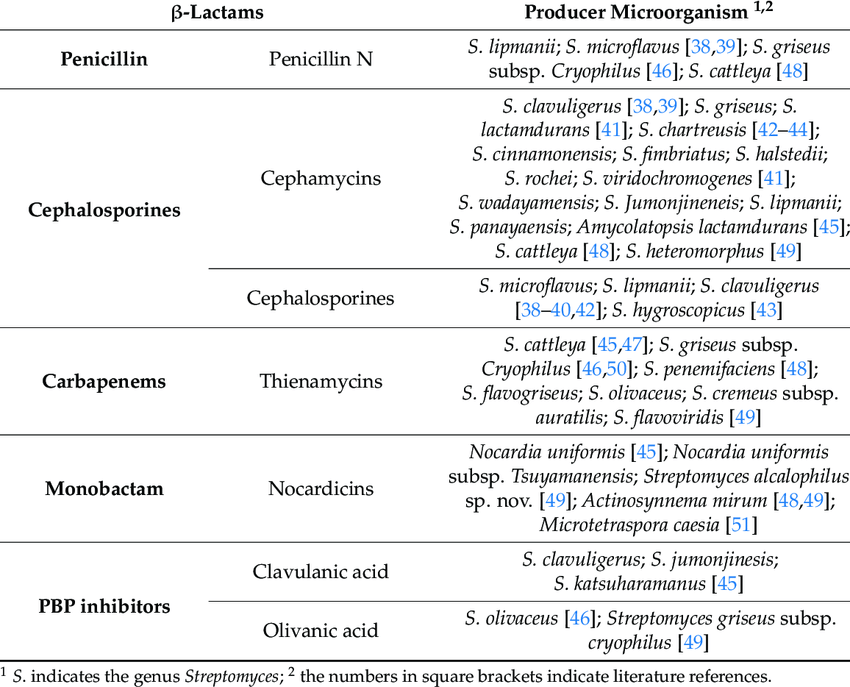
- Penicillins: This class includes penicillin G, amoxicillin, and ampicillin. Penicillins inhibit bacterial cell wall synthesis by binding to and inhibiting enzymes called penicillin-binding proteins (PBPs). This disruption weakens the bacterial cell wall, leading to lysis and cell death.
- Cephalosporins: Cephalosporins, such as cephalexin and ceftriaxone, share a similar mechanism with penicillins, targeting PBPs to disrupt cell wall synthesis. They are often used for more resistant bacteria.
- Macrolides: This class includes erythromycin, clarithromycin, and azithromycin. Macrolides bind to the bacterial ribosome’s 50S subunit, preventing the continuation of protein synthesis. This inhibition ultimately leads to bacterial growth arrest and cell death.
- Tetracyclines: Doxycycline, minocycline, and tetracycline are members of this class. Tetracyclines bind to the bacterial ribosome’s 30S subunit, interfering with the attachment of aminoacyl-tRNA to the ribosome. This prevents the elongation of the growing protein chain.
- Fluoroquinolones: Ciprofloxacin, levofloxacin, and moxifloxacin belong to this class. Fluoroquinolones target bacterial DNA gyrase and topoisomerase IV, enzymes essential for DNA replication and repair. By inhibiting these enzymes, fluoroquinolones disrupt bacterial replication.
- Aminoglycosides: Gentamicin, amikacin, and tobramycin are examples of aminoglycosides. These antibiotics interfere with bacterial protein synthesis by binding irreversibly to the bacterial ribosome’s 30S subunit. This binding leads to misreading of the genetic code and inhibits protein synthesis.
- Sulfonamides: Sulfamethoxazole and trimethoprim are commonly used sulfonamides. Sulfonamides inhibit bacterial growth by blocking the synthesis of folic acid, a key component required for DNA and RNA synthesis.
- Glycopeptides: Vancomycin and teicoplanin are glycopeptide antibiotics that inhibit bacterial cell wall synthesis by binding to the precursor molecules involved in cell wall construction. This prevents the formation of a functional cell wall.
- Oxazolidinones: Linezolid is an oxazolidinone that inhibits bacterial protein synthesis by binding to the 50S subunit of the ribosome. This prevents the formation of functional ribosomes and halts protein production.
These diverse classes of antibiotics showcase the ingenuity of scientists and pharmacologists in developing weapons to combat bacterial infections. Each class targets specific bacterial vulnerabilities, and their combined efforts have led to the impressive success of antibiotics in treating a wide range of bacterial diseases. However, the rise of antibiotic resistance underscores the importance of responsible antibiotic use and ongoing research to ensure the continued efficacy of these invaluable medications.
❖ Antibiotics in Pharmacy Practice
The role of antibiotics in pharmacy practice is multifaceted, extending beyond simple dispensing to encompass critical patient care activities:
- Prescription Review and Consultation: Pharmacists analyze prescriptions for appropriateness, ensuring the correct antibiotic is prescribed, and provide patient education on proper usage.
- Therapeutic Monitoring: Pharmacists monitor antibiotic therapy, ensuring optimal dosing and addressing potential drug interactions or adverse effects.
- Antibiotic Stewardship: Pharmacists play a pivotal role in antibiotic stewardship programs, promoting the judicious use of antibiotics to prevent resistance and preserve their efficacy.
- Patient Counseling: Pharmacists educate patients on proper antibiotic administration, emphasizing the importance of completing the prescribed course and highlighting potential side effects.
- Intravenous Antibiotics: In hospital settings, pharmacists collaborate with healthcare teams to ensure the appropriate dosing and compatibility of intravenous antibiotics.
❖ Challenges of Antibiotic Resistance:

While antibiotics have been a medical marvel, the emergence of antibiotic-resistant bacteria has cast a shadow over their effectiveness.
- Evolution of Resistance: Bacteria have a remarkable ability to adapt and develop resistance mechanisms, rendering some antibiotics ineffective over time.
- Multi-Drug Resistance (MDR): Some bacteria have acquired resistance to multiple classes of antibiotics, severely limiting treatment options.
- Superbugs and Public Health Threats: Resistant bacteria, often referred to as “superbugs,” pose significant public health threats, leading to increased morbidity, mortality, and healthcare costs.
- Overuse and Misuse: Overprescribing antibiotics for viral infections, improper dosing, and patient non-compliance contribute to the development of resistance.
❖ Responsible Antibiotic Stewardship
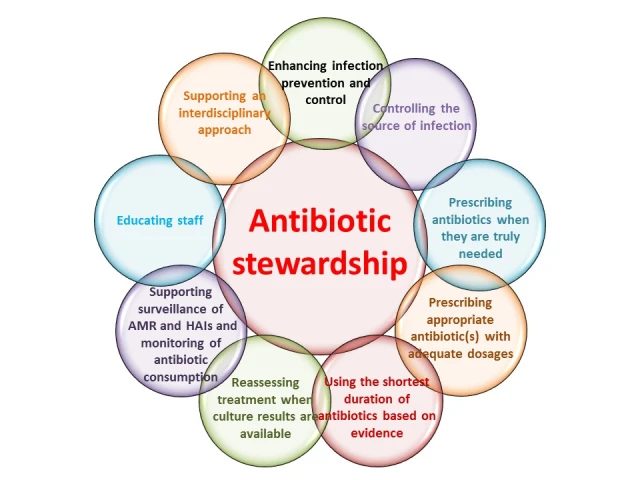
Addressing antibiotic resistance requires a concerted effort from healthcare professionals, policymakers, and patients alike:
- Education and Awareness: Public education campaigns and healthcare professional training are vital to raise awareness about responsible antibiotic use.
- Guidelines and Protocols: Evidence-based guidelines and protocols help guide appropriate antibiotic prescribing practices.
- Pharmacist-Led Initiatives: Pharmacists play a crucial role in antibiotic stewardship programs, ensuring antibiotics are prescribed only when necessary and optimizing their use.
- Developing New Antibiotics: Continued research and development of new antibiotics with novel mechanisms of action is essential to combat emerging resistance.
❖ Conclusion
Antibiotics stand as a testament to human ingenuity and scientific progress, revolutionizing the field of medicine and saving countless lives. In the realm of pharmacy practice, antibiotics serve as indispensable tools, showcasing the pharmacist’s vital role in patient care, education, and antibiotic stewardship. However, the looming specter of antibiotic resistance reminds us of the urgent need for responsible antibiotic use, collaboration among healthcare professionals, and ongoing research to ensure the continued efficacy of these remarkable medications. As we navigate the evolving landscape of antibiotics, let us remember that their responsible use today paves the way for healthier tomorrows.

