❖ Introduction:
Pharmacy is a critical component of healthcare systems worldwide, playing a pivotal role in ensuring safe and effective medication management. Pharmacists are not only responsible for dispensing medications but also for upholding ethical standards and adhering to complex legal regulations. As healthcare continues to globalize, the pharmacy profession faces unique challenges and opportunities in maintaining ethical standards and navigating diverse legal landscapes. In this blog post, we will explore the intricate relationship between pharmacy, law, and ethics in the context of global health, delving into the challenges faced by pharmacists and the opportunities for enhancing healthcare delivery on a global scale.
❖ The Globalization of Healthcare

Globalization has significantly transformed the healthcare landscape, leading to increased access to healthcare services, the sharing of medical knowledge, and the international movement of healthcare professionals and patients. This interconnectedness has presented both challenges and opportunities for pharmacy practice.
❖ Opportunities:
- Information Exchange: Globalization has facilitated the rapid exchange of information and best practices in pharmacy. Pharmacists can now learn from their counterparts in different countries, adapting successful strategies to improve patient care in their own regions. This exchange of knowledge has the potential to enhance healthcare outcomes and promote ethical pharmacy practice.
- Collaborative Healthcare: In a globalized world, pharmacists have the opportunity to collaborate with healthcare professionals from various disciplines and nations. This interprofessional collaboration can lead to more comprehensive patient care, with pharmacists contributing their unique expertise in medication management and safety.
- Advocacy for Global Health Equity: Pharmacists can leverage their position to advocate for global health equity. By working alongside international organizations and local governments, pharmacists can contribute to initiatives that aim to improve access to essential medications and healthcare services for underserved populations worldwide.
❖ Challenges:
- Diverse Regulatory Frameworks: One of the primary challenges pharmacists encounter in global health is navigating the diverse regulatory frameworks governing the practice of pharmacy in different countries. Each nation has its own set of laws, regulations, and standards for pharmacy practice, which can vary widely. This diversity can lead to confusion and potential legal issues for pharmacists practicing across borders.
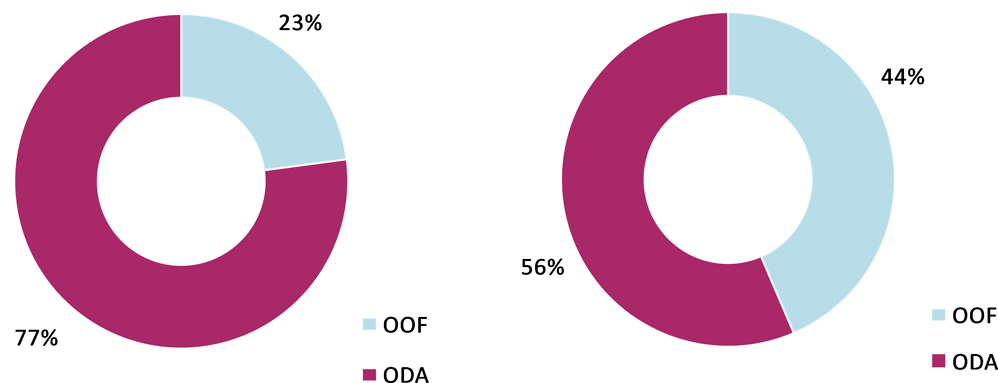
- Medication Availability and Accessibility: Disparities in medication availability and accessibility persist in different parts of the world. While some countries have well-established pharmaceutical supply chains, others face shortages and struggles to provide essential medications. Pharmacists may find themselves in ethical dilemmas when they cannot fulfill their primary duty of ensuring patient access to necessary medications due to supply chain issues or regulatory barriers.
- Cultural and Ethical Sensitivities: Global health initiatives often require pharmacists to work in culturally diverse settings. This can bring to light ethical challenges related to respecting cultural beliefs, patient autonomy, and informed consent. Pharmacists must strike a delicate balance between adhering to their professional ethics and respecting local customs and values.
❖ Challenges in Pharmacy Law and Ethics
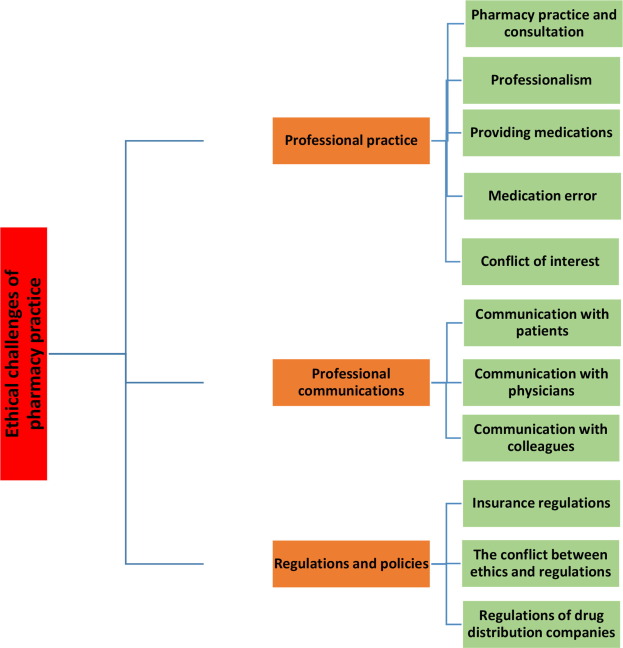
As the pharmacy profession expands its global footprint, pharmacists must grapple with complex legal and ethical issues that transcend national borders. Some of the key challenges include:
- Cross-Border Practice: Pharmacists practicing in multiple countries may face legal challenges related to licensure, credentialing, and liability. Understanding and complying with the laws and regulations of each country in which they practice is essential to avoid legal complications.
- Drug Importation and Exportation: The movement of medications across borders can be subject to strict regulations and may raise ethical concerns related to drug safety, quality, and counterfeit drugs. Pharmacists must be vigilant in ensuring that medications imported or exported meet regulatory standards.
- Informed Consent: Informed consent is a fundamental ethical principle in healthcare, but its interpretation and application can vary across cultures. Pharmacists must be aware of these variations and strive to obtain informed consent from patients in a culturally sensitive manner.
- Ethical Drug Pricing and Access: The global pharmaceutical industry’s pricing and access policies can have profound ethical implications. Pharmacists may be confronted with situations where essential medications are priced out of reach for many patients. Advocating for fair drug pricing and access is an ethical imperative in such cases.
- Pandemic Response: The COVID-19 pandemic highlighted numerous ethical and legal challenges for pharmacists, including vaccine distribution, medication shortages, and emergency authorizations for drug use. Pharmacists played a vital role in addressing these challenges while upholding ethical standards.
❖ Ethical Decision-Making in Global Pharmacy Practice:

Pharmacists practicing in a global health context must navigate these challenges while upholding ethical principles. Ethical decision-making is a critical skill for pharmacists in any setting, but it becomes especially crucial in the complex and diverse landscape of global health. Here are some key principles and frameworks to guide ethical decision-making in global pharmacy practice:
- Autonomy: Respecting patient autonomy is a fundamental ethical principle. Pharmacists should ensure that patients have the information and support needed to make informed decisions about their healthcare, even in culturally diverse settings.
- Beneficence: Pharmacists have a duty to act in the best interests of their patients. This includes advocating for patients’ access to necessary medications and healthcare services, even when faced with regulatory barriers.
- Non-Maleficence: Pharmacists must strive to do no harm to patients. This includes ensuring the safety and quality of medications and adhering to ethical guidelines when faced with challenging situations.
- Justice: Promoting justice in global pharmacy practice involves advocating for equitable access to healthcare resources, including medications. Pharmacists can play a role in addressing healthcare disparities and advocating for fair pricing.
- Cultural Competence: Developing cultural competence is essential for pharmacists practicing in diverse environments. This includes understanding cultural beliefs, communication styles, and healthcare practices that may impact ethical decision-making.
❖ Case Studies in Global Pharmacy Ethics:
To illustrate the practical challenges and ethical considerations in global pharmacy practice, let’s explore two case studies:
Case Study 1: Medication Shortages in a Low-Income Country:
Imagine a pharmacist working in a low-income country where medication shortages are common. The pharmacist is faced with a dilemma: a patient with a life-threatening condition urgently needs a medication that is out of stock. The patient’s family cannot afford to purchase the medication from a neighboring country due to the high cost. What ethical principles should guide the pharmacist’s decision?
In this scenario, the pharmacist must consider the principles of beneficence and justice. While the pharmacist cannot control the medication supply chain, advocating for the patient’s access to essential medication is an ethical imperative. This may involve collaborating with local healthcare authorities, international organizations, and advocacy groups to address medication shortages and promote equitable access to healthcare resources.
Case Study 2: Cultural Sensitivity and Informed Consent
A pharmacist from a Western country is providing healthcare services in a rural village in an African country. The pharmacist encounters a patient with a serious medical condition and recommends a specific treatment plan. However, the patient appears hesitant and does not provide explicit consent for the proposed treatment. The pharmacist suspects that the patient’s reluctance may be due to cultural beliefs and communication barriers. How should the pharmacist approach this situation ethically?
In this case, cultural competence and respect for autonomy are key ethical principles. The pharmacist should take the time to understand the patient’s cultural background, beliefs, and communication preferences. This may involve consulting with local interpreters or healthcare professionals who are familiar with the cultural context. The goal is to facilitate effective communication, provide the patient with the necessary information, and obtain informed consent in a culturally sensitive manner.
❖ Conclusion:
Pharmacy law and ethics in the context of global health present both challenges and opportunities for pharmacists around the world. Navigating diverse legal frameworks, addressing medication shortages, and respecting cultural differences are just a few of the complexities pharmacists encounter in their practice. However, by adhering to ethical principles, advocating for equitable healthcare access, and fostering cultural competence, pharmacists can play a vital role in improving healthcare outcomes on a global scale.

